Dr. Bell is highly trained and experienced in the mechanism of disease that affects the eye. We provide both diagnosis and treatment for most of these conditions. We also have hand picked specialists that we feel are exceptionally skilled at providing specialized care in complex cases. Our services are available 5 days a week. We also provide emergency care when injuries or complications occur in your eyesight. We accept major medical insurance as well as Medicare and Medicaid.
We provide diagnosis, treatment and management of diseases which affect the human eye and visual system. Some examples where we have special training include:


examination.
A cataract is a cloudy or opaque area in the normally clear lens of the eye. Depending upon its size and location, it can interfere with normal vision. Most cataracts develop in people over age 55, but they occasionally occur in infants and young children. Usually cataracts develop in both eyes, but one may be worse than the other.
The lens is located inside the eye behind the iris, the colored part of the eye. Normally, the lens focuses light on the retina, which sends the image through the optic nerve to the brain.
However, if the lens is clouded by a cataract, light is scattered so the lens can no longer focus it properly, causing vision problems. The lens is made of mostly proteins and water. Clouding of the lens occurs due to changes in the proteins and lens fibers.
Cataracts generally form very slowly. Signs and symptoms of a cataract may include:
- Blurred or hazy vision
- Reduced intensity of colors
- Increased sensitivity to glare from lights, particularly when driving at night
- Increased difficulty seeing at night
- Change in the eye’s refractive error
There is no treatment to prevent or slow cataract progression. In age-related cataracts, changes in vision can be very gradual. Some people may not initially recognize the visual changes. However, as cataracts worsen, vision symptoms increase.
Content provided by the American Optometric Association. Click here for more information.
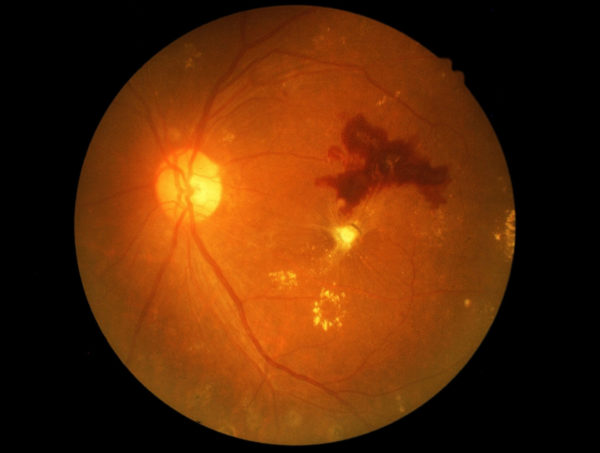 Diabetic retinopathy is a condition that occurs in people who have diabetes. It causes progressive damage to the retina, the light-sensitive lining at the back of the eye. Diabetic retinopathy is a serious sight-threatening complication of diabetes.
Diabetic retinopathy is a condition that occurs in people who have diabetes. It causes progressive damage to the retina, the light-sensitive lining at the back of the eye. Diabetic retinopathy is a serious sight-threatening complication of diabetes.
Diabetes interferes with the body’s ability to use and store sugar (glucose). The disease is characterized by too much sugar in the blood, which can cause damage throughout the body, including the eyes.
Over time, diabetes damages the blood vessels in the retina. Diabetic retinopathy occurs when these tiny blood vessels leak blood and other fluids. This causes the retinal tissue to swell, resulting in cloudy or blurred vision. The condition usually affects both eyes. The longer a person has diabetes, the more likely they will develop diabetic retinopathy. If left untreated, diabetic retinopathy can cause blindness.
Symptoms of diabetic retinopathy include:
- Seeing spots or floaters
- Blurred vision
- Having a dark or empty spot in the center of your vision
- Difficulty seeing well at night
When people with diabetes experience long periods of high blood sugar, fluid can accumulate in the lens inside the eye that controls focusing. This changes the curvature of the lens, leading to blurred vision. However, once blood sugar levels are controlled, blurred distance vision will improve. Patients with diabetes who can better control their blood sugar levels will slow the onset and progression of diabetic retinopathy.
Often the early stages of diabetic retinopathy have no visual symptoms. That is why the American Optometric Association recommends that everyone with diabetes have a comprehensive dilated eye examination once a year. Early detection and treatment can limit the potential for significant vision loss from diabetic retinopathy.
Treatment of diabetic retinopathy varies depending on the extent of the disease. People with diabetic retinopathy may need laser surgery to seal leaking blood vessels or to discourage other blood vessels from leaking. Your optometrist might need to inject medications into the eye to decrease inflammation or stop the formation of new blood vessels. People with advanced cases of diabetic retinopathy might need a surgical procedure to remove and replace the gel-like fluid in the back of the eye, called the vitreous. Surgery may also be needed to repair a retinal detachment. This is a separation of the light-receiving lining in the back of the eye.
If you are diabetic, you can help prevent or slow the development of diabetic retinopathy by:
- Taking your prescribed medication
- Sticking to your diet
- Exercising regularly
- Controlling high blood pressure
- Avoiding alcohol and smoking
Content provided by the American Optometric Association. Click here for more information.
 Dry eyes can be a chronic condition, but your optometrist can prescribe treatment to keep your eyes healthy and comfortable and to prevent your vision from being affected.
Dry eyes can be a chronic condition, but your optometrist can prescribe treatment to keep your eyes healthy and comfortable and to prevent your vision from being affected.
The primary approaches used to manage and treat dry eyes include adding tears using over-the-counter artificial tear solutions, conserving tears, increasing tear production, and treating the inflammation of the eyelids or eye surface that contributes to the dry eyes.
- Adding tears. Mild cases of dry eyes can often be managed using over-the-counter artificial tear solutions. These can be used as often as needed to supplement natural tear production. Preservative-free artificial tear solutions are recommended because they contain fewer additives, which can further irritate the eyes.People with dry eyes that don’t respond to artificial tears alone will need to take additional steps to treat their dry eyes.
- Conserving tears. Keeping natural tears in the eyes longer can reduce the symptoms of dry eyes. This can be done by blocking the tear ducts through which the tears normally drain. The tear ducts can be blocked with tiny silicone or gel-like plugs that can be removed, if needed. Or a surgical procedure can permanently close the tear ducts. In either case, the goal is to keep the available tears in the eye longer to reduce problems related to dry eyes.
- Increasing tear production. Your optometrist can prescribe eye drops that increase tear production. Taking an omega-3 fatty acid nutritional supplement may also help.
- Treating the contributing eyelid or ocular surface inflammation. Your optometrist might recommend prescription eye drops or ointments, warm compresses and lid massage, or eyelid cleaners to help decrease inflammation around the surface of the eyes.
Content provided by the American Optometric Association. Click here for more information.
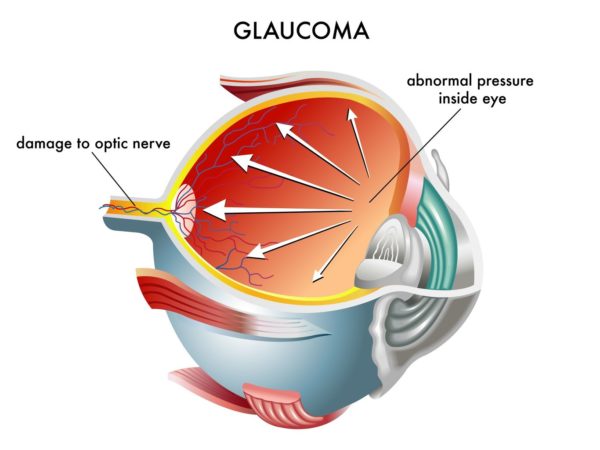
Glaucoma treatment is aimed at reducing pressure in the eye. Regular use of prescription eye drops are the most common and often the first treatment. Some cases may require systemic medications, laser treatment or other surgery. While there is not yet a cure for glaucoma, early diagnosis and continuing treatment can preserve eyesight.
- Medications. A number of medications are currently available to treat glaucoma. Typically, medications reduce elevated pressure in the eye. A single medication or a combination of medications may be prescribed. The type of medication may change if it is not reducing pressure enough or if the patient is experiencing side effects.
- Surgery. Procedures include laser treatment, making a drainage flap in the eye, inserting a drainage valve, or destroying the tissue that creates the fluid in the eye. All procedures aim to reduce the pressure inside the eye when medication is not sufficient. Surgery cannot reverse vision loss.
- Laser surgery. Laser trabeculoplasty helps fluid drain out of the eye. A high-energy laser beam stimulates the structure that drains fluid from the eye (the trabecular meshwork) so that fluid drains more efficiently. The results may be somewhat temporary, and the procedure may need to be repeated in the future.
- Conventional surgery. If eye drops and laser surgery aren’t controlling eye pressure, you may need a trabeculectomy. This filtering microsurgery creates a drainage flap. Fluid can then percolate into the flap and later drain into the vascular system.
- Drainage implants. Drainage valve implant surgery may be an option for adults with uncontrolled glaucoma or secondary glaucoma or for children with glaucoma. A small silicone tube is inserted in the eye to help drain fluid.
Content provided by the American Optometric Association. Click here for more information.
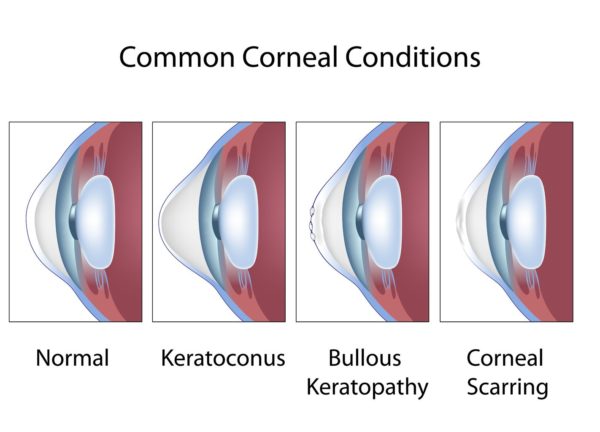 Keratoconus is a vision disorder that occurs when the normally round cornea (the front part of the eye) becomes thin and irregular (cone) shaped. This abnormal shape prevents the light entering the eye from being focused correctly on the retina and causes distortion of vision.
Keratoconus is a vision disorder that occurs when the normally round cornea (the front part of the eye) becomes thin and irregular (cone) shaped. This abnormal shape prevents the light entering the eye from being focused correctly on the retina and causes distortion of vision.
In its earliest stages, keratoconus causes slight blurring and distortion of vision and increased sensitivity to glare and light. These symptoms usually appear in the late teens or late 20s. Keratoconus may progress for 10-20 years and then slow in its progression. Each eye may be affected differently. As keratoconus progresses, the cornea bulges more and vision may become more distorted. In a small number of cases, the cornea will swell and cause a sudden and significant decrease in vision. The swelling occurs when the strain of the cornea’s protruding cone-like shape causes a tiny crack to develop. The swelling may last for weeks or months as the crack heals and is gradually replaced by scar tissue. If this sudden swelling does occur, your doctor can prescribe eyedrops for temporary relief, but there are no medicines that can prevent the disorder from progressing.
Eyeglasses or soft contact lenses may be used to correct the mild nearsightedness and astigmatism that is caused by the early stages for keratoconus. As the disorder progresses and cornea continues to thin and change shape, rigid gas permeable contact lenses can be prescribed to correct vision adequately. In most cases, this is adequate. The contact lenses must be carefully fitted, and frequent checkups and lens changes may be needed to achieve and maintain good vision.
In a few cases, a corneal transplant is necessary. However, even after a corneal transplant, eyeglasses or contact lenses are often still needed to correct vision.
Content provided by the American Optometric Association. Click here for more information.
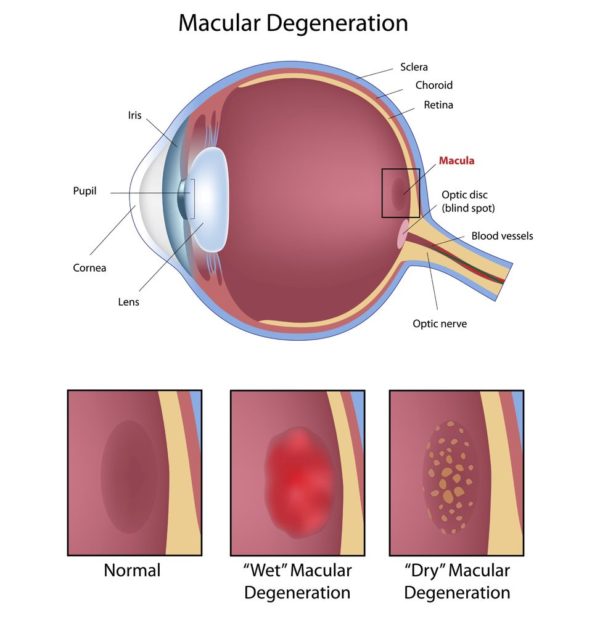
10438066 – eye macular degeneration, eps8
We provide specialized tests to evaluate your personal risks. We can also provide health and nutritional counseling to reduce this risk. In advanced cases, we work closely with specialized Retinal Surgeons who may be needed to treat Macular Degeneration.
In its early stages, the following signs of macular degeneration can go unnoticed.
- Gradual loss of ability to see objects clearly.
- Shape of objects appears distorted.
- Straight lines look wavy or crooked.
- Loss of clear color vision.
- A dark or empty area in the center of vision.
If you experience any of the above signs or symptoms, contact your doctor of optometry immediately for a comprehensive eye examination. Your optometrist will perform a variety of tests to determine if you have macular degeneration or any other eye health problems.
Central vision that is lost to macular degeneration cannot be restored. However, low-vision devices, such as telescopic and microscopic lenses, can maximize existing vision.
Content provided by the American Optometric Association. Click here for more information.